Abstract
Background
Venous thromboembolism (VTE) is one of the leading causes of morbidity and mortality in cancer patients. We investigated VTE prevalence in cancer patients in the emergency department (ED) setting, associated utilization of health care resources and costs.
Methods
The Agency for Healthcare Research and Quality sponsored Nationwide Emergency Department Sample (NEDS) database was used to identify cancer patients and ED utilizations in 2006-12. The NEDS database captures 20% of US ED visits. Cancer types (solid tumor, lymphoma, leukemia, multiple myeloma) and acute venous thromboembolism [VTE, which includes deep vein thrombosis (DVT) and/or pulmonary embolism (PE)] were identified by ICD-9 codes. CPT procedure codes were used to identify any use of computed tomography pulmonary angiography (CTPA), CT chest with contrast (CTC), duplex ultrasound of the veins (DUS), or ventilation-perfusion (VQ) scan. Descriptive statistics were used to present the VTE prevalence, use of imaging study, admission rates and costs incurred. Chi-square test were used to compare death/admission rate and chi-square test for trend was used for trend analysis. Multivariable logistic regression modeling was used to explore the association between VTE diagnosis and hospital admission or death during hospital course after baseline characteristics adjustment.
Results
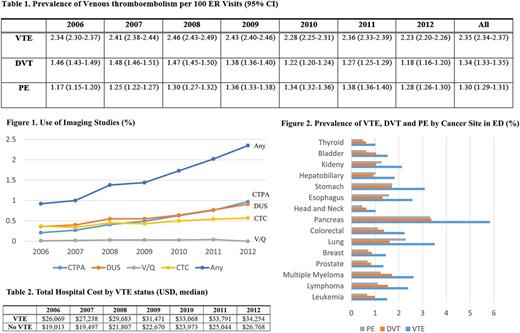
There were 6,330,322 ED visits by cancer patients in our study, which represented 3.2 % of total ED visits from 2006-2012 in the NEDS database. Over the study period, 1.6% of patients received either CTPA, CTC, DUS, or V/Q scan during their ED visits (CTPA: 0.56%; CTC: 0.47%; DUS: 0.62%; V/Q: 0.02%). The use of imaging studies had increased from 0.92 to 2.35 per 100 ED visits (Figure 1, p-value for trend<.0001) over time. The overall VTE rate was 2.35 (95% CI: 2.34-2.37) per 100 ED visits [Table 1, DVT: 1.34 (95% CI: 1.33-1.35) per 100 ED visits; PE: 1.30 (95% CI: 1.29-1.31) per 100 ED visits]. Patients with pancreatic cancer had the highest rate (5.84 per 100 ER visits), followed by lung (3.51 per 100 ER visits) and stomach cancers (3.09 per 100 ER visits) (Figure 2). Patients with thyroid, head and neck and prostate cancers had the lowest rates. Cancer patients with VTE had a higher rate of death in the ED (6.5% vs 4% of those without VTE, p-value<.0001) and a higher rate of admission (92% vs 61% of those without VTE, p-value< .0001). From 2006-2012, the total median hospital cost of cancer patients with VTE increased from $26,069 to $34,254 and were consistently higher than those without VTE (costs: $19,013 to $26,768, Table 2). In the subgroup of patients with solid tumor cancer (N=5,349,246), VTE diagnosis was independently associated with higher odds of admission (adjusted odds ratio (AOR):6.7, 95% CI: 6.56-6.84, p-value< .0001) and hospital death (AOR: 1.24, 95% CI: 1.21-1.27, p-value< .0001) after adjusting for age, cancer types, and metastatic status.
Conclusions
VTE diagnosed in the ED was associated with higher rate of mortality, hospital admissions, and healthcare-associated costs. Imaging studies for VTE are increasingly frequent, suggesting increased awareness by ED providers. Future clinical trials are warranted to investigate the cost-effectiveness of outpatient VTE prophylaxis among cancer patients in order to reduce VTE-associated burden.
Khorana: Halozyme: Consultancy, Honoraria; Janssen Scientific Affairs, LLC: Consultancy, Honoraria, Research Funding; Sanofi: Consultancy, Honoraria; Bayer: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Amgen: Consultancy, Research Funding; Leo: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal